Stress: It’s Not Just “In Your Head”
Get your free guide to stress healing here. Learn how chronic stress may be causing or worsening your illness and what you can do about it.
What is Stress?
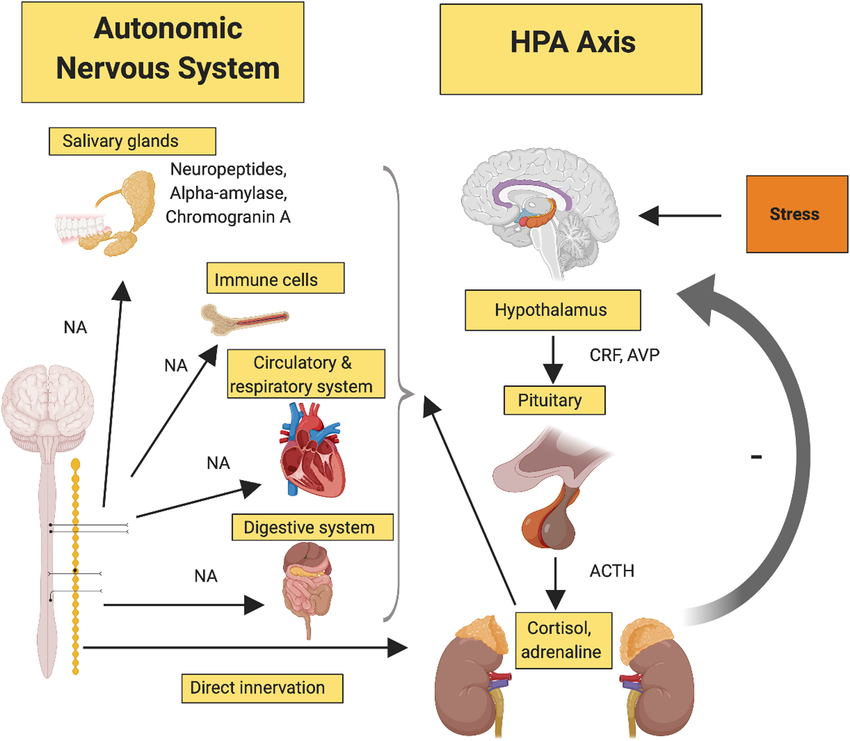
Stress is a physical response that our bodies experience whenever internal or external stimuli called stressors activate the hypothalamic-pituitary-adrenal (HPA) axis. It is an essential survival mechanism that allows the body to respond
to challenges and threats.
The HPA Axis
When the HPA axis is activated, the entire body is effected. In the short term, this acute stress response is protective, preparing the body for fight or flight by releasing glucose into the blood stream, increasing our heart rate and blood pressure to improve blood flow to the brain and muscles, slowing down our intestinal tract, and even reducing inflammation.
However, when stress becomes chronic, the same system can wreak havoc on the body, leading to issues such as fatigue,headaches, gastrointestinal (GI) distress, and even joint pain.
One of the key factors in the transition from acute to chronic stress is the concept of neuroplasticity. This phenomenon explains how the nervous system adapts, sometimes in ways that exacerbate stress and its physical symptoms.
Neuroplasticity: The Nervous System Adapts
Neuroplasticity refers to the nervous system's remarkable ability to adapt and reorganize itself in response to experiences. From the time we’re in our mother’s womb and even into late adulthood, the brain is always adapting and responding to various internal and external stimuli.
Now, when it comes to stress, the center of stress processing lies in the limbic system, a region of the brain responsible for regulating emotions. You’ll note that within this limbic system lies our friend the hypothalamus, the first organ in our HPA axis. Now, as we develop, we typically learn to engage the prefrontal cortex, the logical and conscious part of our brain, which helps us process emotions and regulate our responses to stress. A stimulus enters the brain, and the limbic system is activated, but so too is our logical prefrontal cortex so that we can avoid becoming overstimulated by any and every signal. However, trauma, chronic stress, and other factors can lead to maladaptive changes in neuroplasticity.
These can cause the brain to essentially “skip” involvement of the prefrontal cortex and allow the limbic system to ultimately activate our HPA axis (the organs of the stress response) without our ability to control or sometimes even recognize it. As a result, chronic stress manifests physically, contributing to issues such as persistent pain, headaches, lower back pain, and GI distress. This can affect men and women alive. But something unique happens to women when they experience these maladaptive changes in the nervous system.
Stress and Women’s Health
While stress affects everyone, its impact on women is unique, particularly regarding hormonal health.
The HPG axis
The menstrual cycle is governed by the hypothalamic-pituitary-gonadal (HPG) axis. Once again, there’s our friend the hypothalamus. Now, the HPG regulates the release of follicle-stimulating hormone (FSH) and luteinizing hormone (LH). These hormones act on the ovaries to produce estrogen and progesterone during the menstrual cycle. Chronic stress can disrupt the delicate balance of the HPG axis, leading to menstrual irregularities such as missed periods, heavier flows, or worsened premenstrual symptoms.
Rates of Mental Health Disorders in Women and Men, APA 2017
This disruption doesn't just affect physical health; it can also significantly influence mental health. Compared to men, women generally have more estrogen and progesterone receptors in the brain. This explains in part why women’s moods seem to be sensitive to the different stages in their menstrual cycle. And we see that women are more likely than men to experience conditions like depression, anxiety, and panic disorders, which are often exacerbated by hormonal imbalances caused by stress. To be clear, these mental health concerns are not solely the result of hormonal imbalances, there other factors to consider for sure. But we cannot discount the impact that stress plays psychologically and physiologically on a woman’s mental health.
Additionally, and importantly, stress-related menstrual dysregulation can impact vaginal health and reduce libido. Perhaps most frustrating of all, this dysregulation can exacerbate the already unpleasant symptoms associated with menopause, further influencing overall well-being.
Feel to Heal: Reconnecting the Mind and Body
So, what can be done to restore balance in our body and heal from the effects of stress?
The "Feel to Heal" approach emphasizes restoring the connection between the limbic system and the prefrontal cortex, allowing the brain to better process emotions and regulate the stress response. Effective methods for achieving this include:
Cognitive Behavioral Therapy (CBT): Identifying and challenging negative thought patterns.
Eye Movement Desensitization and Reprocessing (EMDR): Addressing trauma and its effects on emotional processing.
Mindset Coaching: Cultivating a growth-oriented perspective.
Compassionate Inquiry: Exploring the root causes of stress in a safe, nonjudgmental environment.
These approaches require safety, sincerity, courage, consistency, and patience from patients. Safety of course because you need to feel safe enough to explore your emotions and bring up the difficulties of the past. Sincerity because only by being sincere about your emotions can you fully engage your prefrontal cortex in order to help you better understand the stressors that affect you, your emotions, and the impact they’ve had on you. This requires courage, as this can be one of the hardest processes that you engage in. Consistency is key because this is rarely, if ever, something that is resolved in a single session. And you need to be patient with yourself as you walk this difficult path of healing.
Alongside therapeutic interventions, there are practical strategies for managing acute stress, such as:
Breathing exercises: Calming the nervous system through diaphragmatic breathing.
Reframing: Shifting perspectives on stressors.
Exercise: Releasing built-up stress through movement.
Journaling: Gaining clarity and processing emotions by writing.
Confiding in loved ones: Building a supportive network.
The Five Pillars
I tell all my patients, if we could focus on these five pillars of health, I think people like me would be out of business and that would be a good thing. For long-term resilience, the following foundational elements are essential:
Nutrition:
Focus on whole foods, aiming for at least 1.2g of protein per kilogram of body weight daily and 28g of fiber. Minimize processed foods and consider food logging to increase mindfulness.
Exercise:
Incorporate 9-12 multi-joint movements (think push-ups instead of chest fly) weekly with challenging but achievable effort. Strive for 150 minutes of moderate-intensity cardiovascular activity each week. Moderate intensity means it’s challenging and requires you to focus on your breath during the activity.
Sleep:
This is HUGE! Prioritize 7-8 hours of quality sleep. Maintain a consistent sleep routine and avoid screen time before bed.
Relationships:
Cultivate meaningful connections. Identify at least three people you can trust and work on communication
and boundary-setting.
Spirituality:
Reflect on your personal identity and purpose through three guiding questions: Who am I? What does that mean for my life? How does the way I'm living now compare to my answers?
These five pillars address everything that makes us human and the fundamental needs that we have to
maintain a healthy life.
Summary
Stress may be a natural response, but chronic stress can severely impact mental, physical, and hormonal health, particularly for women. By understanding the mechanisms behind stress, such as neuroplasticity and its effects on the HPA and HPG axes, we can take steps to mitigate its impact. Approaches like "Feel to Heal" and strategies focused on acute stress management, combined with attention to the Pillars of Health, provide a comprehensive roadmap for reclaiming well-being.
Stress isn't just "in your head"—it's in your body, too. With the right tools, it's possible to break the cycle and promote healing from within. And as always, if you’re in the Fayetteville, NC area and you’re looking for a primary care practitioner who takes these things in consideration when working with patients, you should reach out! At TrueCare DPC I love to take a holistic approach to medicine, taking into account the delicate connection between the mind and the body and all things that make us human. Email me at golfran@truecaredpc.com
References
1. Ball, Jake & Darby, Ivan. (2022). Mental health and periodontal and peri‐implant diseases. Periodontology 2000. 90. n/a-n/a. 10.1111/prd.12452. Access on November 19, 2024 at https://www.researchgate.net/figure/Effect-of-stress-on-the-hypothalamic-pituitary-adrenal-HPA-axis-Activation-of-the_fig3_362396854
2. Crevoshay, Eve & Sawyer, Sarah & Kowert, Rachel & Boccamazzo, Raffael & Dunlap, Kelli & Cocks, Jane & Skimmons, Ryan & Kocurek, Carly & VanDenBogaard, Jay & Rogers, Lisa. (2019). State of the Industry 2019: Mental Health in the Game Industry. Accessed on November 19, 2024 at https://www.researchgate.net/profile/Kelli-Dunlap-
2/publication/336208930/figure/fig1/AS:849860148346880@1579633857063/The-effects-of-chronic-stress-according-to- McEwen-2006.png
3. Raikar, S. Pai. Limbic System. Encyclopaedia Britannica. Accessed November 20, 2024. https://www.britannica.com/science/limbic-system.m.
4. Holmes M. Menstrual Cycle Phases. Tampax Accessed August 12, 2024. https://tampax.co.uk/en-gb/period-health/menstrual-cycle-phases/
5. Hayden M. Your Menstrual Cycle: The Basics. Women's Health Network. Accessed November 20, 2024. https://www.womenshealthnetwork.com/pms-and-menstruation/your-menstrual-cycle-the-basics/
6. 1.EFP Clinic. Hormonal Causes of Infertility: Module 1 Fertility Information. Accessed November 20, 2024. Enhanced Fertility Programme. Hormonal imbalance. Accessed on November 20, 2024 at https://efp.clinic/course/module-1/module-1-fertility-info/info-hormonal-causes/
7. Richards M, Van Neil M. Mental Health Facts for Women. American Psychiatric Association.. Published April 2019. Accessed November 20, 2024. https://www.psychiatry.org/getmedia/aa325a61-5b60-4c71-80f1-dc80cf83c383/Mental-Health-Facts-for-Women.pdf